British Medical Casualties on the Western Front in the Great War Part 1: Dealing with Wound Related Trauma
- Home
- World War I Articles
- British Medical Casualties on the Western Front in the Great War Part 1: Dealing with Wound Related Trauma
British Medical Casualties on the Western Front in the Great War Part 1: Dealing with Wound Related Trauma by Dr David Payne
(This article first appeared in Stand To! 83 August / September 2008 pp. 27 - 32)
Introduction
When confronted with the onset of the Great War in August 1914, the professional British Regular soldier, and his colleagues in the Reserve would have had no illusions about the dangers of the battlefield. He was also well acquainted with the high mortality rate that battle injuries caused and that this was often due to the rudimentary level of wound surgery, and the after care, that was available on and off the battlefield. Also, he would have been aware of the spectre of wound infection; not least of which was the deadly gas gangrene (caused by the bacterium Clostridium perfringins) for which, once the disease was established, there was no effective treatment other than radical surgery.
For the volunteer soldiers (aka Service men) and the Territorials, who did not have the Regular soldiers’ prior battlefield experience, perhaps the threat would not have been so stark and evident. Due to the British practice of the immediate burial at sea of naval casualties and the interment of fallen soldiers on, or close to, the battlefield where they fell, virtually none of the dead were transported home. Consequently there were no huge military cemeteries such as the Arlington National Cemetery in Washington, USA, to catch the public’s attention. Its one square mile of 300,000 serried headstones, dating back to May 1864, has constantly served to remind the American public at large of the heavy cost of war.
Also, whilst some crippled ex-soldiers certainly existed in Britain prior to the outbreak of war in 1914, not many were seen on the streets, as was the certainly the case post-1918.
Battle casualties in conflicts prior to the Great War, although relatively high as a percentage of the participants, were usually quite low in numbers compared with what was to occur in the almost incessant fighting on the Western Front. Here there was a daily average of 5,000 deaths with a total casualty count on all fronts in excess of 11 million. Even the cataclysmic Battle of Waterloo in 1815 only produced 15,000 British casualties. Whilst the first day of the Battle of the Somme, on the 1st July 1916, alone produced 60,000 British casualties; of which 20,000 were killed. Another 360,000 British casualties were to follow as the Somme battle raged on until heavy snowfalls in November 1916 reduced the fighting to the level of local skirmishing. (The preciseness of some of the casualty figures often quoted for the various battles of the Great War belies the state of chaos and delay under which they were usually compiled and the admittedly limited clerical resources usually available to properly collate them. Here figures are rounded to more realistic approximations).
Moreover, in the earlier wars, the period that a soldier expected to be under fire, and in mortal peril, was much less. It is said that even the most famous and highly decorated British soldiers of the past had only spent a total of 24 hours, or so, actually under fire in their entire careers. During the Great War, such a period of exposure to intense warfare could be experienced by a British soldier in a single tour of duty ‘in the line’.
Similarly, the pre-1914 British Regular and Reserve soldier would be well aware of the swathes that were regularly cut through the ranks of the army by various epidemics and plagues that they encountered across the world during their service. The volunteer and Territorial soldier, on the other hand, would probably only be aware of a low level, but fairly constant, toll of illness in his homeland. This constant occurrence of death due to illness was a normal part of life in north-western Europe at that time, although it mainly affected the youngest segment of the population – the infants and other children under fourteen, where up to 50 percent died in childhood - and the aged population. On the other hand, pneumonia was known as ‘the old man’s friend’ as it terminated many a life blighted by the chronic diseases of the aged.
Of course, no one had the slightest inkling of the devastation which would be caused by the influenza epidemic that, in the last year of the Great War, would selectively strike down huge numbers of the serving soldiers’ age group on the Western Front and elsewhere across the globe. It was the greatest pandemic (ie worldwide epidemic) since the bubonic plagues of the Middle Ages up to the present day (see also Stand To! 67, April 2003, p.16).
The processing of medical casualties on the Western Front
The formation of the Royal Army Medical Corps (RAMC) on 23 June 1883 by Royal Warrant, and the associated reorganisation in 1902 of the Army Nursing Service into the Queen Alexandria’s Imperial Nursing Service, had allowed the British Army’s medical services to be put on a more professional and effective basis. There was also a new Royal Army Medical College at Woolwich and a school of sanitation at Aldershot that for the first time oriented the army’s approach to the practice of good hygiene both on and off the battlefield. In particular, the preparation of sterilised drinking water was formalised and the means established of transporting this potable water supply to all the soldiers in the field. By 1914, all these new procedures were well established throughout the British Army.
A further reorganisation that had greatly affected the role of the army medical officer on the battlefield was the creation of the Field Ambulances and Field Hospitals. (In this context the Field Ambulance (FA) was a RAMC mobile medical unit with a strength of ten officers and 224 other ranks; later increased from early 1915 with another officer and twenty-five ORs who formed the Sanitary Section). The FA was charged with the collection, treatment and clearance of the wounded and the sick from the environs of the battlefield and for mobility purposes was usually housed in tents.
When the British Expeditionary Force (BEF) left for France in August 1914, on its strength were nineteen RAMC Field Ambulances – three for each of the six divisions and one for 19 Brigade. As indicated earlier, each BEF FA was responsible for the clearance of casualties from the field from a brigade area in the front line by means of their collection from Regimental Aid Posts (RAP) and other casualty concentration points. The FA provided these casualties with immediate medical treatment as necessary and, as indicated by their wounds/illness, ensured their onward transfer to the Casualty Clearing Station (CCS). Ultimately, the more serious cases entered the Base Hospital organisation that extended back to the UK; an amazing 40 percent of the wounded/sick were repatriated to the UK during the conflict.
Whilst initially the role of ‘camp followers’ on the Western Front was practically nil in 1914, as the Great War progressed increasing numbers of ‘other nationalities’ - Chinese, Black South Africans, Egyptians and Indians for example - were employed in Labour Corps with numbers reaching some 150,000 in 1918. Special medical facilities were required to care for them. Inevitably, the further up the Lines of Communications these workers were employed, the greater the numbers of battle trauma casualties that occurred. In the event, considerable numbers of these casualties had to be repatriated to their respective Homelands for various reasons.
The range of battlefield trauma
When the BEF arrived in France in August 1914, the generals, the politicians and the general public alike anticipated a short war; ‘Home by Christmas’ was the slogan.
Based on experience in the Boer War fought twenty years previously, the War Office expected that the medical services would have to deal with about 5 percent of the total soldiery suffering from trauma wounds. They also assumed that there would be an unpredictable, but significant, number of casualties due to the communicable diseases that were always associated with men at war. Although the range and efficacy of lethal weaponry had increased since the Boer War along with the impact of the new high explosives, the generals still thought the majority of wounds would arise from bullets and shrapnel balls. They also allowed that there would be some injuries due to the shrapnel shells themselves, and their explosive effect, and the sabre, bayonet and the lance of which the latter two weapons, although relatively rarely deployed, produced surprisingly high fatality rates. (In 1914 the British had practically no high explosive/splinter fragmentation type shells in their armouries). In short, the majority of the soldiers’ wounds would be of the simple penetrating type associated with open warfare; later in the war the lacerating wounds from the splinters of fragmentation shells, mortars and grenades became the majority. Of course, even when the simple missiles such as bullets or shrapnel balls struck bone, serious and complicated injuries could arise. The kinetic effect of even the standard rifle/machine gun round used in the Great War (not ‘dumdum’ or ‘tampered’) is often under-estimated. Leaving the barrel at 2,700 feet per second, if one struck the cranium of the skull it would usually totally destroy the brain and a limb-bone could be badly splintered beyond repair. In the case of such wounds to the limb-bones this could necessitate amputation and its associated complications.
In the event, within a very short period after the outbreak of hostilities, open warfare quickly became untenable due to the level of lethality it assumed. The troops of the belligerent nations went to ground into a massive 460-mile long subterranean creation of barbed wire, trenches, dugouts and fortifications. Had the troops not done so, the enormous casualty rates associated with open warfare and modern weapons would have probably brought the war to an inevitable early end: the fighting armies would have literally run out of troops fit to fight.
To deal with this radically changed scenario, machine guns became much more numerous, and produced an unprecedented range of multiple wounds. Also, high explosive fragmentation (splinter) shells, mortars and hand-grenades became the norm inflicting partial and total dismemberment and other mutilation injuries. In addition, crush and asphyxiation injuries became common as trenches and dugouts collapsed onto their occupants under heavy and prolonged shelling using high explosive.
By the spring of 1915, toxic gas had been introduced by the Germans and became a major cause of disablement, if not proportionally leading to many deaths. As the war progressed the use of toxic gas in various forms, kinds and presentations became almost universal along the Western Front.

Struggling through. Stretcher bearers bringing a wounded man over muddy ground at Passchendaele, 14 November 1917. IWM CO 2202
Medical Statistics
Perhaps for the first time in a major conflict, many more Great War soldiers were to die from wounds than did from disease, ie a ratio of 5:1. However, contrarily, there was a considerable drop in the numbers of Deaths from Wounds and that 55 percent of these occurred whilst the servicemen were under medical care in casualty clearing stations or other field medical units. The remainder died further up the treatment chain, confirming an improved system of patient care from that which pertained in the Boer War. A similar improvement occurred in the ‘ill and injured’ category.
At the outbreak of the Great War in 1914 no plans had been made for the systematic collation of medical statistics and, indeed, no provision had been made for the attachment of a responsible administrative medical officer to the Staff of the Commanding Officer, BEF. Only in November 1914 were clerical and statistical staff officially assigned to medical statistical duties. Moreover, as mentioned earlier, the provision of these resources was rarely generous enough to meet all requirements competently in a rapid and standardised way. So, precision in the casualty records from the early part of the Great War should be viewed with some suspicion and approximations are the wisest course. It was only in June 1917 that standardised recording procedures were adopted universally by the War Office and funding regularised, although it is considered that only the Western Front records of the British Expeditionary Force actually achieved this university of application.
Post-war, further efforts were made to rationalise and collate all the Great War medical records for statistical and pensions purposes; particular attention being made to casualty numbers, manpower resources and wastage.
Breakdown in battle trauma statistics
Comparative analyses of the primary weapons of the Great War on the Western Front shows that the bullet (rifle and machine gun) produced 39 percent of casualties, shells and other missiles 59 percent, hand thrown bombs and grenades 2 percent and bayonets/lances less than1percent. More exotic weapons such as flame-throwers and tanks produced relatively low numbers of casualties although they possessed a strong shock effect, particularly when first introduced.
The distribution of the site of wounds receiving medical treatment is somewhat surprising at first analysis: 39.3 percent of the wounds occurred in the feet and legs; 31.0percent in the hands and arms: 17.1 percent in the face, head or neck; 6.5 percent in the back; 3.9 percent in the chest and 2.3 percent in the abdomen. Moreover, flesh wounds accounted for a massive 79.3 percent of all the wounds that received medical attention and many more received unrecorded self-treatment.
The emergency treatment of wounds
Each active service soldier was provided with an emergency field dressing; larger shell dressings were available within the infantry platoon. They were basically cotton bandages to which were attached wads of cotton wool treated with a microbicide. A safety pin was provided to secure the dressing in place over the wound. In use they were effective at staunching most non-arterial blood flows and for keeping the wound relatively clean until appropriate treatment was available. Unfortunately, major infection into the wound often occurred during the moment of trauma, and it was this deeply embedded detritus that later caused so much trouble. (See Gangrene below). However, the simple, emergency field dressings had an important psychological affect in reassuring the wounded soldier that he was being medically cared for and to a certain extent that he could provide first aid for himself should the need arise.

A high risk of infection. An Australian officer wades through Gird trench, Guéudecourt, late1916. Conditions were so atrocious in this area during the early November fighting that the Australian official historian Charles Bean described them as ‘the worst ever known to the First AIF’. IWM E (AUS) 572
Surgical practice on and off the battlefield
Fortunately, throughout the Great War the anaesthetic chloroform and the strong analgesic (painkiller) morphine were in good supply to the British surgeon. So once a soldier did get to a source of trained medical care he could be sure of an adequate level of pain relief. The French soldiery was less fortunate and they suffered from frequent shortages of both analgesics and anaesthetics on the battlefield.
As the war increased in intensity and scope on the battlefield, greater availability of morphine to the wounded was ensured even at the furthest front line level. Otherwise, in 1914, the British military medical officer and surgeon had a rather limited armamentarium of remedial measures that he could employ to give succour to the wounded. (There were increasing numbers of female physicians and surgeons during the Great War but no female doctors were commissioned in the RAMC). His interventions were haunted by the spectre of infection and shock; it took a courageous surgeon to step outside the officially recognised procedures. Moreover, at the outset of the war, surgery was only attempted at the Base Hospital level and that necessitated often long and painful transportation for the wounded soldier from the battlefield. In the early months of the war, for example, chest surgery was limited to the drainage of pus and the surgical handling of the organs of the thoracic cavity was considered to be hazardous in the extreme. Consequently, the making of the necessary surgical incisions to permit the removal of foreign bodies, or for the suturing of internal chest wounds, was generally discouraged at the cost of many lives.
By the end of 1916, the reality of the casualty situation, as was most forcefully demonstrated by the military disaster that was the Somme Offensive, obliged a rethink on the deployment of medical care facilities both on, and close to, the battlefield. Proper surgical teams were formed with the necessary back-up medical staff and other facilities. Accordingly, these teams were introduced much closer to the front line and a speedier and efficient flow of the wounded was created. This resulted in greatly shortened transport times and a reduction in the suffering and trauma that the wounded experienced en route.
Also a more adventurous attitude was adopted in relation to the treatment of wounds. Blood transfusions were introduced, as were X-rays. Tissue debridement (surgical removal of flesh and muscle) was more aggressively applied, early forms of plastic surgery were practised and active cleansing and draining of infected wounds generally instituted. More strenuous efforts were also made to remove foreign bodies and close open wounds as soon as possible, as was the immobilisation of fractured bones by wooden splints (the Thomas Splint) and other supportive means. All these measures greatly enhanced survival rates and gave better recovery and rehabilitation outcomes.
These more favourable rates also proved to be a considerable factor in the ability of the belligerent nations to keep the fighting going despite the horrendous casualty rates: the British claimed over 80 percent of their wounded were returned to duty; some on several occasions.
Two doctors from London hospitals – Sir George H. Makins and Sir Anthony A. Bowlby - were appointed as medical consultants to the British Army. They instigated much of the more progressive changes in medical practice that took place in the BEF during the Great War.
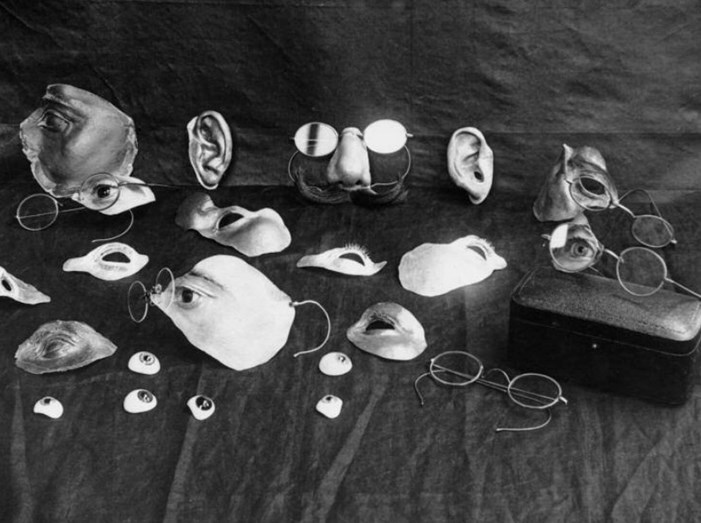
Repairing war’s ravages. Items used to disguise facial injury during the early development of plastic surgery. Included are eyes, ears, noses and parts of the face, as well as several pairs of spectacles, which were used to disguise the joins and keep some parts in place. This photograph was probably taken at 3rd London General Hospital, Wandsworth. IWM Q 30460
The dreaded gangrene duo and tetanus
One of the greatest and more intractable medical problems faced by the medical organisation on the Western Front were the two conditions known as dry and wet gangrene. The latter of these two infections was often associated with a frequently fatal condition called lockjaw, which, as the name describes, produces a symptomatic fixation of the facial muscles. Without recourse to modern antibiotics and other supportive measures, the treatment of either type of the gangrenes was largely based on aggressive surgery allied with intensive nursing care. Dry gangrene: When the circulation of the blood is seriously affected in an injured or diseased area – usually on the extremities - the affected tissues are subject to deterioration and, at worse, necrosis (death). Unless circulation can be effectively reinstated, the only solution is rigorous debridement of tissue, or amputation of the entire limb. Later in the Great War concomitant infestations of wounds by fly maggots – Phormia/Phaenicia spp. and others - were observed by US Army Surgeon William Baer et al to be highly efficient in the debridement process, as they attacked only dead and damaged tissue and simultaneously sterilised the wound. Unfortunately, this promising therapy was not developed until after the Great War but it is still in use today. The fungal disease associated with exposure to cold, wet conditions that caused the condition known as Trench foot led to many amputations due to gangrenous complications. Wet gangrene: This was an even more serious problem, and led to innumerable deaths of wounded soldiers. As mentioned earlier, it was caused by a bacteria -Clostridium perfringens - along with other anaerobic (living in an oxygen-free environment) bacteria that are commonly found in heavily manured agricultural soil. In the rural areas of France and Belgium wounded soldiers were infected by contact with the infected soil, particularly through mud caked uniforms: even the dirty straw that was widely found in soldiers’ barracks, billets and first aid centres could be a source of the infection.

Foot inspection. Returning from a spell in the front line, men of 10 Australian Brigade have a foot inspection at Dragon Farm Passchendaele, 1917. IWM E (AUS) 939
Once introduced into a deep wound these anaerobic bacteria rapidly produce gas. This further opens up the muscle fibres and associated tissue and allows even more invasion of the adjacent tissue. Also, large quantities of powerful toxins are produced which seriously damage the infected tissues and the adjacent healthy tissue. The result is a rapidly developing area of necrosis that, unless speedily arrested, can readily cause toxic shock and death. Radical surgery, including amputation of the infected digit or limb, is frequently the only option and many of the Great War soldiers’ amputations were due to this cause. Where amputation was impossible, radical surgical debridement of tissue was the only alternative course of action.

‘Gassed’. British troops line up for treatment at a dressing station near Bethune, 10 April 1918. The famous painting ‘Gassed’ by John Singer Sergeant shows a scene very similar to the photograph. IWM Q 11586
Tetanus: The bacteria Clostridium tetani are also found in heavily manured soil and quickly establishes itself in penetrating wounds. It produces a deadly toxin for which there is no neutralising antidote. About 50 percent of those who demonstrate symptoms die a painful death. In September/October 1914, the British Army introduced a preventative tetanus inoculation, but tetanus cases still occurred in the trenches of the Western Front with fourteen hospital admissions in 1915 (equivalent to 2 per 100,000 of the BEF serving on the Western Front) and five deaths. Subsequently, the number of tetanus cases was reasonably contained despite the huge increases in the numbers of British and Dominion troops on the Western Front. In 1916 there were 254 admissions (19 per 100,000 strength) and 146 deaths; in 1917, 271 admissions (14 per 100,000 strength) and 134 deaths, and in 1918, 112 admissions (6 per 100,000 strength) and 59 deaths. Accordingly, at the end of the War admissions for and deaths from tetanus in the British and Dominion members of the BEF on the Western Front represented an extraordinary success against this battlefield scourge. The main innovator of this preventive inoculation work was Sir David Bruce, a much-acclaimed British military expert in tropical diseases.
Toxic gas
The introduction by the Germans of the poisonous gas chlorine on a large scale onto the Western Front in April 1915 posed a whole new set of problems for the military physician and surgeon both on and off the battlefield. Chlorine was released as a gas from high compression steel cylinders – dubbed ‘Oojars’ by the British – via a system of pipes that were routed over, or through, the parapet of the trench and so aligned that the toxic gas would be blown by a favourable wind into the Allied trenches. Depending on the concentration achieved (one part per million in air was the putative threshold of toxicity) the toxic gas produced numerous lung and mucous membrane affected casualties. (Chlorine gas in contact with the water in the lungs and the mucous membranes produces hydrochloric acid that is highly corrosive).
Initially, there were no protective anti-gas masks and clothing against the toxic gas, and many soldiers died an agonising death. But the Allies acted with great speed and energy and within days ad hoc protective masks were deployed on the battlefield. Other more effective devices quickly followed. By the autumn of 1916 the British had produced a ‘box respirator’ that was highly effective against chlorine gas if promptly and properly deployed.
Later, even more devastating gases such as phosgene (late1915) and mustard gas (1917) were widely used by both sides. These gases were delivered by gas shells or other suitably designed missiles. Mustard gas also affected moist unbroken skin raising huge painful blisters. This latter gas, delivered in liquid form, often lingered for days contaminating whole areas of the battlefield and, occasionally, beyond.
Eventually, special British Divisional Gas Treatment Centres were set up on the Western Front, as were gas casualty clearing stations and hospitals specialising in the treatment of gas cases. Numerically, the notified British toxic gas admissions to hospital for the war after 1915 were comparatively low – around 190,000 representing around 10 percent of the total British wounded hospital admissions, and the mortality rate proportionally lower still – around 6,000. Nevertheless, gas-warfare was generally considered by both sides as the one of the more horrid and mutually hated aspects of the War.
By and large, the treatment that was available for exposure to toxic gas was mainly palliative and the degree of recovery largely depended on the recuperative power of the gassed soldier. Many seriously gassed soldiers were affected for the rest of their lives, particularly with pulmonary (lung) problems. However, of those admitted to hospital as a gas casualty (93 percent of those presenting to casualty clearing stations), around 94 percent subsequently returned to duty.
Treatment of psychological trauma
Although by definition the condition known as ‘shell shock’ is not strictly a ‘wound related trauma’, no survey of the treatment of battle trauma on the Western Front would be complete without at least a reference to this serious ailment.
Throughout history there have been reports of nervous disorders associated with long military campaigns and sieges; often referred to by euphemisms such as ‘Nostalgia’ (Swiss mercenaries), ‘Longing for home’ (Germans), ‘Da Costa’s Syndrome’ (Americans – Civil War) and ‘Neurasthenia’ (British). However, as early as 1914 on the Western Front, during the Battle of Mons and the subsequent Retreat, considerable numbers of the British Expeditionary Force were found to be suffering from ‘a serious mental disability’ sufficiently acute to prevent them performing their duties effectively on active service. It was particularly notable that the majority of these men had not received any serious battlefield injury, thus rendering the then supposed causative reason of ‘proximity to an exploding shell(s)’ as, at best, dubious. Also, in the class-oriented attitudes current in those days, officers were thought to suffer from a different condition from their men. Officers’ symptoms were said to be due to overwork and the heavy burden of responsibility they bore in war. Hence the terms ‘Effort Syndrome’ and ‘Disordered Action of the Heart’ that was exclusively applied to officers.
The officer class indubitably faced considerable physical stress in performing their battlefield duties and generally bore a very heavy burden of responsibility that by itself inevitably led, in a few cases, to mental breakdown. But the main cause of their mental and physical collapse was closely related to that affecting their men, that is, various forms of combat fatigue or stress.
From the time the term ‘shell shock’ was first used by Dr Charles S. Myers on the Western Front in 1915, it quickly came to be widely used by the soldiery and general public alike. However, for some time the medical officer cadre preferred such official terms as ‘Concussional, or Commotional, Shell Shock’ or ‘Nervous Shock or Emotional Stress’. By the end of the Great War the general nature of ‘shell shock’ was more clearly understood by all concerned and most civilians too had met, or heard of, BEF soldiers suffering from the condition.
However, during the conflict on the Western Front, it took considerable time and bureaucratic vacillation for the British military authorities to come to terms with this problem of battle stress, and even when they did, some commanders continued to treat it as a military discipline problem. These officers reacted accordingly, with, at worst, cases occurring of patently shellshocked soldiers being executed for cowardice: decisions that resonate in the conscience of many of the British public to this day.
Eventually, special facilities were created to deal with the shell shock problem, and this led to an increasing emphasis on treatment ever closer to the battlefield.
While the problem of shell-shock was never ever fully solved and eliminated in the Great War, or since, the total number of British shellshocked soldiers reported as being invalided out of the British Army on a pensionable basis was only 50,000; although these figures are disputed by some authorities as being far too low. (Many of these pensions were reviewed periodically post-war by the Board of Control of the Ministry of Pensions and subsequently annulled as the soldiers’ health was said to have improved).
However, there certainly was some success in the rehabilitation of the shell-shock cases during the Great War and, reportedly, overall, 75 percent were returned to duty. However, 80 percent of those actually hospitalised with the condition never returned to duty. Also, treatment greatly improved as the war progressed: after the Third Battle of Ypres (Passchendaele) in 1917, 50 percent of shell shock cases were rapidly returned to their units, whilst another 20 percent were returned to duty after a two month period of convalescence away from the battlefield.
Post-war, many of the lesser shell-shock cases were lovingly brought back to some normality in the bosom of their family with very little, if any, state support. However, a considerable number of them were never to fully recover, neither within, nor outside, health institutions, and affected men were to be seen in every walk of life for many years. Members of the general public are reported as making comments such as, ‘Around here, since the men came home, it is like a lunatic asylum.’ In 1929, ten years after the end of the conflict, there were still 65,000 shell-shock cases hospitalised in Britain.
Postscriptum
It is not commonly realised what a serious drain the treatment of the British casualties of the Western Front had on the health care structure of the home country during the Great War. From the first, there was the requisition of many of the prominent British health facilities for use in the treatment and rehabilitation of the wounded and sick soldiers, airmen and seamen. Also, most critically, the supply of medical doctors for the Western Front was almost entirely obtained from those employed in public and private health care across the UK and the Empire. By the end of the hostilities, 50 percent of all the UK’s 22,000 medical doctors had volunteered for, or been conscripted for duty on the Western Front. The impact this had on the medical care of the civilian population can be readily imagined. But it was just another example of how the British population on the Home Front shared at least some of the deprivations suffered by the men on the Western Front.
There was also a small, but significant, drain on the homeland medical resources as some of the then relatively few female UK qualified medical doctors volunteered for service with the armies of the Triple Entente (Britain, France and Russia). Most did so under the aegis of the International Red Cross Movement as they were largely shunned by the British War Office, particularly so in the early days of the Great War. One such well qualified applicant – Dr E. M. Inglis - who subsequently rendered outstanding service to the war effort of the Allies - was advised thus by a War Office official, ‘My good lady, go home and sit still.’
References
This article is based on many sources, primary and secondary, with many of the books now out of print, hard to find outside of the National Archives, or expensive to buy. However, patently the most useful source on this subject is Medical Services, Casualties and Medical Statistics, by T.J. Mitchell and G.M. Smith. 1931 (Reprinted 1997 and published by the Imperial War Museum, London, England and The Battery Press, Nashville, USA). At the time of writing both versions were out of print but copies may still be obtained through specialists such as Abebooks.co.uk as new or second hand.