Malaria in the Great War
- Home
- World War I Articles
- Malaria in the Great War
A 1946 map by kind permission of the World Health Organisation)
Malaria in the Great War by Dr David Payne
(This article first appeared in Stand To! No.77 September 2006 pp5 - 8)
Introduction
Throughout history pestilence has been the cause of the majority of the casualties of war. In general, the Great War proved to be an exception, with a ratio of deaths in action versus deaths due to disease of 5:1. However, on some Fronts (e.g. East Africa and Salonika), not even the combined effect of the machine gun and high explosive could equal the casualty roll due to sickness, of which malaria was often a significant part.
Malaria and its vector
Malaria is found in many animals including man. It is transmitted from a sick to a healthy man by the mosquito - the vector of the disease.
Malaria is a disease of the red blood cells (RBCs). The RBCs are destroyed by the malaria parasite as it consumes the contents of these sack-like cells, the haemoglobin. Haemoglobin - its colour makes the blood red - transports around the body the oxygen necessary for the sustenance of all the cells. The process of the destruction of huge numbers of RBCs by the malaria parasites eventually causes the symptoms of malaria fever (sweating), rigour (shivering) and anaemia (pallor). If a sufficient number of parasites invade the RBCs, they can overcome the immune defences of malaria patient and he, or she, will die; often quite rapidly. Even if the patient should recover from the attack of malaria, there may be a long convalescence, or even long term disability with the obvious deleterious effect on fitness for active service.
The malaria parasite is very small, growing from 1 to 20 microns in diameter (i.e. one million to 50,000 per linear inch). When mature it much resembles the amoeba studied in biology classes at school. Its scientific name (Genus) is Plasmodium and there are four species that attack humans: Plasmodium malariae, Plasmodoium vivax, Plasmodium ovale and Plasmodium falciparum. The distribution of malaria is focused on the tropical countries but some species can occur in temperate countries; due to Global Warming there are fears it will even return to southern England where, as the Ague, it was well reported in historical documents
Around 80% of all malaria cases that occur worldwide do so in Africa south of the Sahara. Accordingly, most indigenous Africans have a high degree of immunity and that, as we shall see, made them much more effective as soldiers in the Great War Campaigns in Africa.
The vector, or carrier, of the disease from person to person is a mosquito of a particular Genus - (Anopheles). The species of the vector mosquito varies from continent to continent (e.g. Africa: Anopheles gambiae) and often differs from country to country.
The mosquito transmits malaria from a person suffering from the disease to a healthy person in several stages. First, the mosquito sucks up the blood of the sick person containing the RBCs infected with the malaria parasite. Then, inside the mosquito body, the parasite develops into an invasive form and concentrates in the mosquito's salivary glands. When the malaria infective mosquito bites a healthy person, it injects the anti-bloodclotting saliva containing the parasites into a blood vessel of the healthy person, and draws up their blood into its stomach. Some of the malaria parasites will not be sucked up by the mosquito and will escape into the healthy person's blood system. There they infect new RBCs and begin to rapidly multiply. After some days, enough RBCs have been infected for the patient to develop the symptoms of malaria. If the patient is not treated quickly enough with the appropriate antimalarial drugs, the patient will suffer from malaria and may die.
Malaria and the military
It is no coincidence, therefore, that the discoverers of the cause of malaria and the carrier of the disease were both military surgeons serving in tropical countries. Armies have always been plagued by malaria epidemics (sudden periodic increases in malaria cases) and, more recently, army doctors have been given the responsibility of preventing or curing the infection, as was to be the case in the Great War.
Even in peacetime in the early part of the 20th Century, British Army units serving in tropical countries could routinely expect an annual hospitalisation rate due to malaria of around 350/1000 troops, and 700/1000 was by no means exceptional.
The malaria parasite was discovered with the microscope in 1880 by a French Army doctor (medecin-major), Charles Louis Alphonse Laveran (1845-1922) serving in Algeria with the French Army. He was studying a sick French soldier's blood seeking the cause of his high fever.
The role of the malaria-carrying mosquito was discovered by a British Army surgeon Ronald Ross (1857-1932). Ross was working in Calcutta, India in 1897, and after innumerable experiments in many kinds of mosquito, he found the malaria parasite Plasmodium developing in the body of an Anopheles mosquito.
Malaria, the disease, was well recognised by army doctors and for centuries had been treated by am extract from the bark of a South American tree - the Cinchona Tree. The ground-up bark was called 'The Jesuits Powder' as for many years the Jesuit Order used it, and guarded the secret of its source. A crystalline extract was obtained later (1820) from the bark and was called quinine.
After the discovery by Ross, the various military authorities devised methods for mosquito control and, at least in principle, during the Great War systematically treated soldiers with quinine (five grains - 300 milligrammes - per day) whenever they were thought to be at risk in malarious countries. The colonial expatriate officers got so used to the astringent taste of their daily preventive dose of quinine dissolved in gin that they added a small amount of quinine to soda water to replicate the taste in one of their social drinks - gin and tonic.
Malaria and the Great War
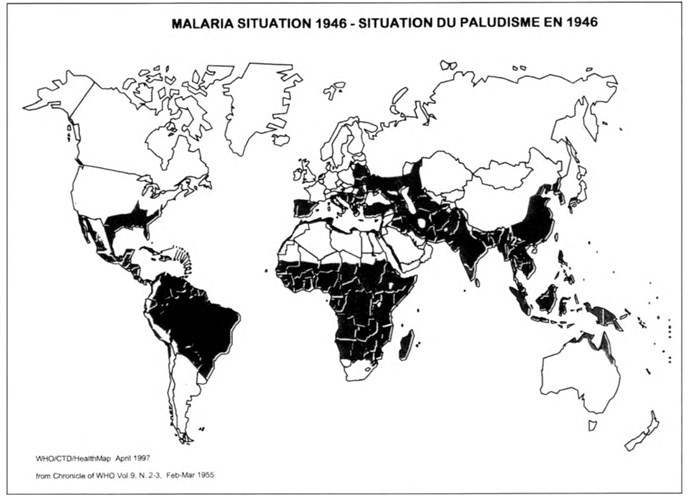
A look at a malaria distribution map at the outbreak of war in August 1914 would have revealed that a huge swathe of the countries then, or later, involved in the fighting were classed as malarious. They were located in two bands around each side of the Equator. A 1946 map (p. 6: by kind permission of the World Health Organisation) reveals a similar pattern.
The inner, tropical, band was about 2000 miles wide on either side of the equator, with the exception of areas covered by desert or high altitude terrain (2,500m+). These are areas where the Anopheles vector mosquitoes could not flourish due to the absence of water (for breeding places) or too a low temperature and/or humidity. Accordingly, Plasmodium faciparum, or tropical malaria, was found almost everywhere in this tropical band where the temperature ranged from 20-30 degrees Celsius and the humidity was 60%+. Accordingly, Plasmodium faciparum, or tropical malaria, was found almost everywhere in this tropical band where the temperature ranged from 20-30 degrees Celsius and the humidity was 60%+.
In addition, Plasmodium malariae, Plasmodium vivax and Plasmodium ovale occurred at a much lower prevalence and were more sporadic. But Plasmodium vivax was largely absent from large parts of the African continent as the indigenous sub-Saharan Africans were genetically immune to it, so there was no reservoir of parasites to support transmission.
As mentioned earlier, around 80% of all of the global malaria cases now occur in tropical Africa south of the Equator and 90% of all the Plasmodium falciparum cases are found there. The situation during the Great War was probably very much the same.
In the Northern Hemisphere another band of malaria transmission extended to the extreme north as far as North America, much of southern Europe, Southern Asia and the Japanese Islands. In this area malaria was less intense and increasingly seasonal the further north one went. The maximum latitude at which malaria transmission was recorded was 64 degrees North at Archangel, Russia. Epidemics occurred in the years when the weather pattern was more favourable to the vector mosquito.
Plasmodium vivax was particularly found in the temperate regions outside the tropical band, whilst P. falciparum was rather rarer due to the lower ambient lower temperature that it could not tolerate. All malaria parasites cease to develop in the mosquito at temperatures less than 16 degrees Celsius.
In the Southern Hemisphere the second band was much narrower, but extended into South America (maximum latitude was 32 degrees South at Cordoba, Argentina), Southern Africa and Northern Australia and some of the Pacific Islands.
Another problem faced by the military of all the belligerent nations was that many war zones became more favourable to malaria epidemics because:
Malaria-infected soldiers from malarious countries were introduced in large numbers into an area where there was a potential for the transmission of malaria. In the same area there were large numbers of non-immune soldiers who were highly susceptible to the disease. After the end of the Great War, returning British soldiers who had served in malarious areas 'introduced' malaria, to Southern England and 500 cases of malaria occurred in the civilian population.
The hugely disruptive effect of war could be highly favourable to the increase in mosquito numbers. The normal man-made, or natural, means of mosquito control were interrupted, and huge numbers of water-holding excavations and containers were created that were favourable for mosquito breeding. Domestic animals, which normally provided the preferred feeding sites for mosquitoes, were distributed elsewhere or destroyed, and the huge numbers of potential human feeding sources took their place.
Treatment of malaria
By definition, the regimentation and innate discipline associated with an army on active service in the Great War made the provision of malaria treatment and prevention measures a much easier task than that which could be achieved in a less controlled civilian population.
Nevertheless, an efficacious treatment regimen for malaria was always dependent on the proper administration of an appropriate antimalarial drug in good time. The only effective treatment for malaria from 1914-1918 was the drug quinine. The source of the drug was limited to mainly South America, the Dutch East Indies, India and East Africa, so for some belligerent nations obtaining adequate quantities of the drug was often difficult.
Faced by such a supply problem, the German East African army produced its own quinine at its Research Institute at Amani, in the Usambara Mountains in Northern Tanganyika - now Tanzania. Thus, it was able to maintain the efficacy of its European German officers and NCOs in the field from 1914-1918, despite the British blockade of medical supplies.
In addition, quinine had side effects. One of these was tinnitus (a persistent ringing in the ears) which many patients found difficult to tolerate over the full seven days or so of the treatment, while other distressing side-effects were giddiness, blurred vision, nausea, tremors and depression. Whenever possible patients were hospitalised to ensure compliance with the full regimen of treatment, even if the patient felt fit enough to leave hospital. The cumulative effect of these long hospitalisations could be crippling on military strength at crucial times in the fighting.
Another, much more life threatening side effect was a disorder called Black Water Fever, so named because of the black coloured urine produced by the patient. It was a result of a complex reaction of the haemoglobin of the patient's RBCs with the malaria parasite Plasmodium faciparum and the drug quinine. Up to 40% of Black Water Fever cases died, and under arduous conditions of war the death rate was often significantly higher.
The War Zones and the distribution of malaria in the Great War
Although the Great War was indeed global in terms of the participation of nations, in terms of the areas of the actual fighting and massing of troops, it was far less so.
There was no land fighting in North and South America, Antarctica and much of Asia and Africa.
Even in Europe, only part of France and Belgium was directly involved in the trench and more open warfare, plus the northern part of Italy/south-western part of AustriaHungarian Empire, the Balkans, the Caucasus part of the Russian Empire and the adjacent states.
In the Middle East fighting was limited to parts of North Africa, Egypt, Turkey (The Dardanelles), Palestine, Transjordan, Mesopotamia and Persia.
In Africa it was restricted to the German colonies in East, West and Southwest Africa and, in part, to the adjacent countries.
There were also limited military operations against German colonies in the Pacific Ocean, Australasia and China.
The role of malaria in these War Zones can be summarised as follow
The Western Front: France and Belgium There were outbreaks of malaria in the France and Belgium (and also other European countries) during 1914-18, but these were thought to be mainly due to introduced malaria, as was mentioned earlier:
On the actual Western Front, malaria could have been theoretically present on a strictly seasonal basis in the areas of lowlying land, as the vectors were present. But the ground was so torn up and polluted by men, munitions and toxic gas that the potential breeding places were largely unsuitable for the Anopheles vector species. Even if the Anopheles mosquitoes had managed to get a foothold, the usually more aggressive non-malarious mosquitoes, better adapted to breeding in polluted water, would probably have crowded them out. Accordingly, despite the presence of very large numbers of potential malaria carriers in the hundreds of thousands of troops that came from Africa and Asia, and served on the Western Front in various capacities, there was little opportunity for malaria transmission of any of the Plasmodium species on the Western Front.
So, while there were outbreaks of malaria in England, France, Belgium, Holland and Germany, there were no epidemics on the Western Front during the Great War.
The Italian Front: Italy and Austria-Hungary
In the early part of the 20th Century the Roman hinterland was notorious for its summer malaria epidemics. But the war zone was limited to the north in the Trentino Valley and the River Isonzo plateau along the Italian/AustroHungarian Alpine border. Most of the fighting took place in the foothills of the Alps, where the main health hazard was the winter rain, cold and snow avalanches. Malaria when it occurred was sporadic and limited to the river valleys.
The Balkan Front: Greece, Bulgaria, Serbia, Albania, Montenegro, Dalmatia, Bosnia-Herzegovina, Slovene, Thrace and Macedonia.
Throughout history, the country around the Danube and its tributaries as it passed through Romania, Serbia, Bulgaria, and the Thessalia and Peloponissos plains in southern Greece, had been noted for seasonal epidemics of malaria.
In 1916-17 a concentration of over 500.000 British, French and Serbian troops was based in Salonika (Macedonia) when an epidemic of malaria broke out in the town, which became to be known as the 'Bird Cage', and its environs. Of the 300.000 British and French troops, around 120.000 (40%) became unfit for active service due to malaria. Allied with other diseases, at one point it reduced the strength of the Allied force to only 100,000 effectives.
In the 1918 battles, through Bulgaria to the Danube, there were only 200,000 battle cases compared with the 450,000 men who had been invalided out of the area suffering from malaria, or its aftermath. Out of the total Allied force of one million who were in the theatre from the end of 1915 to 1918, there were 1.3 million hospital cases, mainly malaria. In the Autumn of 1916, the French Commander of the Expeditionary Force, General Maurice Paul Emmanuel Sarrail, sent a telegram to Army HQ in Paris 'Mon armee est immobilisee dans les hopitaux' (My army is hospitalised'.) The casualties of the Central Powers in the war zone were also dramatic, but reportedly considerably lower: probably due to its forces holding the healthier higher ground, allied with better anti-malarial drug regimens and disease control measures.
The Caucasus Front: Georgia, Azerbaijan, Armenia and Anatolia Although malaria vectors were present in this area and malaria did occur during the summer months, there were no epidemics from 1914 to 1918.
The Eastern Front: Provinces of the Russian Empire - Livonia, Kurland, Lithuania and Poland, East Prussia and Austria / Hungary-Galicia All were malarious, with the plains, lakes and swamplands of Hungary, along with its eastern borders with Romania and Serbia, being particularly associated with seasonal outbreaks most years. But no serious epidemics were reported during the war years although, paradoxically, just after the war there was a Russian pandemic that spread through the Caucasus and Central Asia. It is reported that 600,000 people died of malaria in the region and Plasmodium falciparum cases occurred as far north as Archangel.
The Middle East: Egypt, Palestine, Turkey, Syria, Mesopotamia In all of the Middle East countries involved in the Great War during the malaria season, there was a steady flow of malaria cases to be treated with a peak from June to September. The areas around the Nile in the Sudan and Egypt, and those adjacent to the Tigris and Euphrates in Mesopotamia had regional epidemics that inevitably involved the Armies fighting there.
In Palestine, by the end of 1918, half of the Australian-led Desert Mounted Corps was incapacitated with malaria and 100 died.
The malaria situation in Mesopotamia and the Gallipoli Peninsula was notable for several reasons. In Mesopotamia, the 1916-17 the campaign by the British Indian Tigris Corps, and other British/Indian/ANZAC units, took place along the two great river systems of the Tigris and Euphrates. These rivers produced innumerable breeding sites suitable for the malaria vectors and malaria transmission. Additionally, after the surrender at Khut A1 Amara, on 3 April 1916, the 12,000 survivors of General Sir Charles Townshend's 6th Indian Division were incarcerated under very grim conditions. There was very little provision for malaria prevention, or treatment, and many of the POWs succumbed to malaria alone, or to a complex of other tropical diseases, malnutrition and malaria.
The Dardanelles: Although the Allies' occupation of the beaches of Gallipoli lasted barely nine months, it included the malaria season of 1915 and the Gallipoli Campaign was particularly noted for its high number of malaria cases along with other tropical diseases. Of the 480,000 Allied troops on Gallipoli, 90,000 were evacuated due to sickness, many due to malaria.
The Pacific Islands: The small operations carried out in islands such as the Carolines and Marianas by the Australian and New Zealand Navy and Army, did not present any difficulty with malaria as they were located in a malaria-free area: there were no malaria vector mosquitoes. However, German New Guinea was an entirely different matter as it was in the equatorial zone of high transmission.
The African Campaigns: All of the colonial armies in Africa were beset by the problem of the lethal tropical diseases that thrived there - in particular in the forests and savannahs of sub-Saharan Africa around the Equator, where malaria transmission occurred throughout the year. During the various campaigns in Africa the overall ratio of sick to battle casualties was over 300:1.
Consequently, all of the armies (except those of German Southwest Africa) on both the German and Allied sides were increasingly comprised of black African mercenaries or conscripts - called Askaris - who were largely immune to the lethal tropical diseases including malaria. The Askaris were led by an ever-reducing nucleus of disease-wracked Europeans kept relatively malaria-free by daily doses of quinine.
Also, all the armies depended on a vast corps of African bearers, or porters. They were essential to convey the kit, food and munitions of the front-line troops across the almost trackless bush and forest; in East Africa alone the British employed over a million. Whilst most of the porters were immune to malaria, there was still a high wastage due to desertion, other tropical diseases, infections and malnutrition; a death rate of 20% was the norm in both East and West Africa. Likewise, beasts of burden were soon decimated by zoonoses (animal diseases), such as sleeping sickness carried by the tse tse fly. It is significant that the Germans generally had a much higher ratio of porters to soldiers - 7:1 - than the Allies - 4:1 - and a higher standard of disease prevention, both of which led to significantly lower disability rates in the fighting troops and the porters.
It was the difficulties experienced by the Germans in obtaining sufficient quantities of quinine to supply all their tropical war-fronts that inspired them to search for synthetic alternative antimalarial drugs. This in turn increased their later prominence in malaria pharmacology world-wide.
German West Africa - Togoland - was situated in one of the most highly malarious areas in the world, with-year long transmission of three of the human malarias including the most severe - Plasmodium falciparum. Over the previous century, West Africa had rightfully earned the sobriquet of 'The White Man's Grave' and falciparum malaria was one of the major reasons why there was very little permanent European settlement in this part of Africa. Accordingly, only eight members of the 600 strong defence force were German. Also the vast majority of the 600 British and 200 French invading forces were respectively West African troops of the West African Frontier Force and Senegalese Askaris. Since the campaign in Togoland only lasted from 6-26 August 1914, its brevity and the malaria immune status of the African troops of both sides, meant malaria was not a serious problem.
German South West Africa was largely coastal desert and high savannah, with malaria mainly concentrated around the Owambo and Caprivi Strip areas in the extreme north, adjacent to the Angolan border. Accordingly, the purely European German Colonial Army of 3,000 managed to hold out against the South African General Smuts' 12,000 strong Southern Group, and a Rhodesian contingent, until 17 July 1915 without employing any Askaris; although there was the usual complement of bearers and porters. There was some sickness, including malaria: out of the 266 South Africans who died during the campaign, 156 succumbed to disease and accidents.
German East Africa - Kenya, Tanganyika - and the adjacent nonGerman countries, all had high levels of malaria mainly concentrated along the coastal plain bordering the Indian Ocean, around the Great Lakes of the Rift Valley - eg Lakes Victoria and Tanganyika - and the Zambesi river system. However, malaria was also found on the hinterland plateau below 2,500m, albeit more seasonal and epidemic in nature.
It is somewhat surprising to the impartial observer to find that the Germans appear to have had a clearer understanding of the problems of fighting a war in tropical Africa with malaria nonimmune troops than the experienced colonist British. From the outset the Tanganyikan Askaris formed 75% of the ultimately 15,000 strong German East Africa Colonial Army (the Schutztruppe). Even the large contingent of British/Indian troops in the British Expeditionary Force fell under the curse of rampant Plasmodium falciparum malaria, although the disease occurred in epidemic form on the sub-Continent
British and Empire troops suffered enormous numbers casualties due to malaria during the fouryear campaign with 51,000 of the British forces hospitalised with malaria between June and December 1916 alone. Of the South African contingent alone, 12,000 troops had to be repatriated with malaria by the end of 1916. It was only by an increasing use of malaria-immune African troops from East, Southern and West Africa that it was possible for the British to bring the East African campaign to a successful conclusion in 1918.
The control of malaria on the Great War battlefronts Apart from the use of quinine as a malaria preventative and a curative, other means to control the transmission of malaria were used by the armies of all sides.
Since Ross's discovery in 1897 of the chain of malaria infection through the mosquito, attempts had been made around the British cantonments and encampments of the world to reduce both the numbers of the mosquitoes breeding in water and the airborne adults. One anecdotal Great War control measure was reported from Salonika, where it is said the bushes, and the air itself, were beaten with leafy branches in an attempt to reduce the swarms of mosquitoes.
With the clear understanding that epidemics of malaria were often associated with concentrations of troops, various more effective malaria control measures were employed by the belligerent armies. Prime amongst these were drainage schemes to eliminate the mosquito larvae breeding places, and the use of mosquito bed nets and netting to prevent mosquitoes from biting - malaria vector mosquitoes mainly feed at dusk, during the night and at dawn.
Also less common at the time, was the application of insecticides, such as mineral oil for the water-borne mosquito larvae, and a knockdown pyrethrum spray - an extract of the Chrysanthemum spp. plant mixed with kerosene oil - for the adult mosquito. The pyrethrum spray was known to the British and Americans as ‘Lefroy's Liquid'. Other more readily available toxic products were used ranging from carbolic acid to chlorine gas. All these measures were expensive, by the values of the time. This, plus the difficulty of widespread application and the contingencies of war, limited their use on the battlefield.
In the better organised of the Great War armies, the control of malaria became part of the duties of the long established Regimental Sanitary Squad (RSS), under the direct supervision of the Regimental Medical Officer (RMO), or the equivalent. Personal protection measures, other than the use of the bed nets, and the enforced wearing of veiled hats, long sleeved shirt/jackets, long trousers and mosquito boots, were rather limited. They mainly required the use of mosquito repellent oils, such as Citronella (a lemon scented oil extracted from South Asian grass Cymbopogon nardus) which was generally considered as being the most efficacious.
The willingness and ability of the various Great War armies to obtain and distribute such 'luxury' antimalarial items on a sufficiently wide scale as to be generally effective varied considerably. But it was never an easy task under active service conditions
Postscript
Malaria was never a clear war-winning or war-losing factor in the Great War. But in certain war zones it played a considerable influence on the duration of the campaign, the total casualty list and the composition of the armies that were required to fight in the more highly malarious zones.
During the Great War, the European Armies certainly learned that unless they could provide low toxicity anti-malarial drugs and efficient protection technology against adult mosquitoes, European, and other non-immune soldiers, could not fight a long campaign in a malarious area, especially one within the Plasmodium falciparum distribution range. Until such preventative and curative practices were available, the bulk of the fighting in these highly malarious countries had to be done by naturally immune soldiers, like black Africans.
Elsewhere, if non-immune troops had to be deployed in malarious areas, a sophisticated and flexible hospital care system had to be established. It would have to meet a rapid influx of cases when malaria epidemics struck, almost at random, so that the sick troops could be treated before complications set in, and * they could be speedily returned to active service to maintain military strength.
As the German Army demonstrated in several theatres of war, use of malariaimmune troops, good hygiene discipline and appropriate medication could make a vital difference between success and failure for an army in the field.